Introduction
Human Microbiome: Ever heard the saying, “You’re not just what you eat, you’re what you host”? Welcome to the fascinating world of the human microbiome. It’s a bustling community of trillions of microorganisms living inside and on your body and they’re not just along for the ride. These microscopic allies are critical to your digestion, immunity, mood, and even how your body responds to medications. Let’s break down the microbiome from the ground up and discover why it’s being hailed as one of the most important discoveries in modern health science.
What Is the Microbiome?
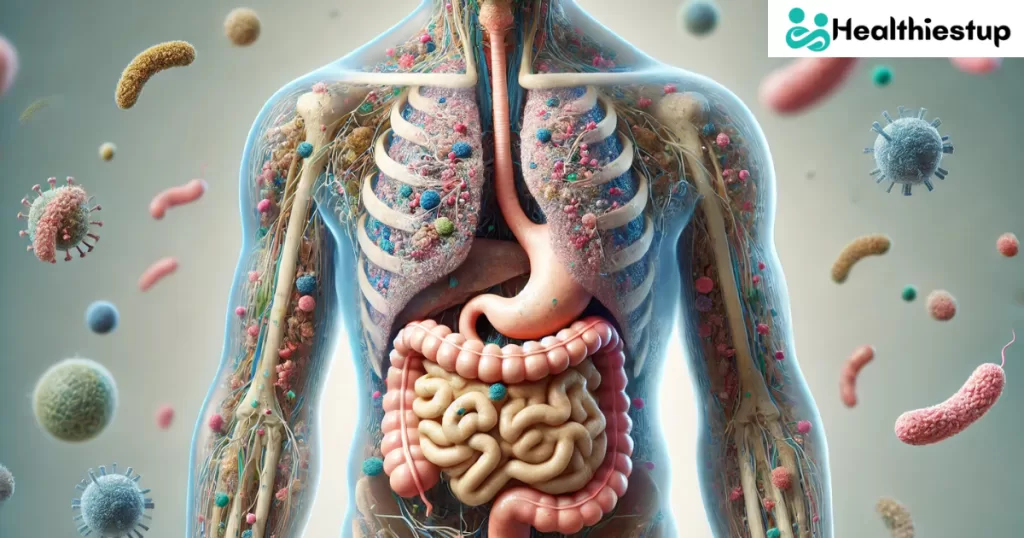
Human Microbiome: The human microbiome refers to the full collection of microorganisms bacteria, viruses, fungi, and protozoa that live in and on our bodies. These microbes outnumber human cells in our body, and the largest population resides in the gut, particularly in the large intestine. But the microbiome isn’t limited to the gut; it also exists on your skin, mouth, lungs, and even reproductive organs.
Think of your microbiome as a rainforest. Just like a rainforest, it thrives on diversity. Each species has a role some break down food, others produce vitamins, and some protect you from harmful invaders. When this ecosystem is balanced, you feel energized, resilient, and healthy. But when it’s out of whack? That’s when problems start creeping in.
This unique system is shaped by factors like birth method (vaginal vs. C-section), diet, antibiotic use, lifestyle, and even your pets. And the best part? You can influence it. Yes, the way you eat, live, and move can directly impact the richness and diversity of your microbiome.
The Gut Microbiome: Your Internal Powerhouse
Human Microbiome: Among all the microbiomes, the gut microbiome is the superstar. It houses more than 70% of your immune system and plays a vital role in digesting fiber, synthesizing vitamins like B12 and K, and managing inflammation. The bacteria here feed on the food you eat especially prebiotic-rich foods like garlic, onions, bananas, and oats and in return, they produce beneficial short-chain fatty acids (SCFAs) that keep your gut lining healthy.
What’s wild is that your gut is sometimes referred to as the “second brain.” Why? Because of the gut-brain axis a two-way communication system between your gut and brain. The microbiome influences neurotransmitter production, like serotonin and dopamine, which affect mood, focus, and even sleep. If your gut is unhappy, chances are your mind is too.
But when the gut microbiome becomes imbalanced a state called dysbiosis you can experience bloating, fatigue, skin issues, weight gain, autoimmune diseases, and even mental health disorders like anxiety and depression. That’s how important this microbial metropolis really is.
Skin Microbiome: Your First Line of Defense
Human Microbiome: Let’s not forget the skin your largest organ. It’s covered in billions of bacteria that protect against pathogens, control inflammation, and maintain the skin barrier. This “shield” helps your skin stay hydrated, youthful, and strong.
The skin microbiome changes depending on the part of the body. Oily areas like the forehead and nose host different microbes than dry areas like elbows. And just like your gut, it can be thrown off by things like harsh soaps, antibiotics, poor diet, and stress.
Imbalances here can lead to acne, eczema, rosacea, and infections. That’s why more skincare products are now focused on being microbiome-friendly. Probiotic and prebiotic skincare is becoming the new frontier helping restore and feed the skin’s good bacteria.
The Oral and Respiratory Microbiomes
Human Microbiome: The mouth isn’t just where digestion starts it’s also a microbial hotspot. A balanced oral microbiome can protect against cavities, gum disease, and even bad breath. But disruptions can lead to oral infections and increase the risk of diseases like endocarditis (a heart infection) and complications in pregnancy.
Similarly, your respiratory tract especially the nose and lungs also has its own microbiome. A healthy balance here can reduce your risk of respiratory infections, asthma, and allergies. Researchers are now exploring how lung bacteria affect diseases like COVID-19, COPD, and lung cancer.
What’s interesting is how these systems are all interconnected. A problem in your gut can reflect on your skin. Oral imbalances can impact heart health. It’s all part of one massive microbial network.
Why the Microbiome Matters for Your Immune System
Human Microbiome: Here’s the truth: your immune system wouldn’t function without your microbiome. These tiny organisms help “train” your immune system to differentiate between friend and foe. Early in life, exposure to diverse microbes helps prevent autoimmune diseases and allergies by building tolerance.
Your gut microbiota plays a critical role in immune signaling. It tells immune cells when to activate, when to calm down, and what to attack. That’s why overuse of antibiotics especially early in life can disrupt this balance and increase the risk of autoimmune conditions and chronic inflammation.
Probiotic-rich foods like yogurt, kefir, and kimchi can help replenish the good guys. But more importantly, feeding your microbiome with a fiber-rich diet keeps it flourishing. It’s about nurturing, not nuking, your bacteria.
The Microbiome and Mental Health: The Gut-Brain Connection
Human Microbiome: Have you ever felt “butterflies” in your stomach when nervous or had a “gut feeling” about something? That’s not just metaphor it’s biology. Your gut and brain are in constant communication through the vagus nerve, hormones, and neurotransmitters. This system is known as the gut-brain axis, and the microbiome is right at the center of it.
Gut microbes influence your mood, behavior, and cognitive function. They help produce neurotransmitters like serotonin (about 90% of it is made in the gut), dopamine, and GABA, all of which play roles in regulating emotions and mental health. When your microbiome is in balance, it acts as a buffer against stress and anxiety. But when dysbiosis hits, it can trigger inflammation that affects your brain function leading to symptoms of depression, anxiety, and brain fog.
Emerging research even links gut microbiome imbalances with neurological conditions such as Alzheimer’s disease, autism spectrum disorder, and Parkinson’s. Scientists are now exploring “psychobiotics” probiotics that support mental well-being. Foods like fermented vegetables, yogurt, and high-fiber plants are not just good for your belly they might also boost your mood.
How Diet Shapes Your Microbiome
Human Microbiome: You are what you feed your microbes. The fastest way to shape your microbiome is through your diet. What you eat can either feed beneficial bacteria or nourish harmful ones. Diets high in sugar, refined carbs, and processed foods promote inflammation and support pathogenic bacteria. On the flip side, a diverse, plant-rich diet filled with whole grains, legumes, fruits, vegetables, nuts, and seeds encourages microbial diversity and that’s the golden ticket to good health.
Prebiotics (found in foods like garlic, onions, leeks, and asparagus) are types of fiber that feed your beneficial bacteria. Probiotics (like those found in yogurt, kefir, sauerkraut, and miso) introduce live bacteria into your system. And then there are postbiotics beneficial compounds like SCFAs that microbes produce during fermentation, which support gut lining and immune regulation.
Want a thriving microbiome? Eat the rainbow. Variety is key. Aim for 30+ plant types a week, drink plenty of water, and limit antibiotic overuse and chemical-laden products that can disrupt your internal ecosystem.
Antibiotics: Friends or Foes?
Human Microbiome: Antibiotics can be lifesaving, but they come with a catch. They don’t discriminate they kill both good and bad bacteria. A single course of antibiotics can wipe out a significant portion of your gut flora, and in some cases, it may take months (or even years) for it to recover fully.
The overuse and misuse of antibiotics whether through prescriptions, livestock in meat production, or antibacterial soaps have led to an alarming rise in antibiotic-resistant bacteria. Even worse, frequent antibiotic exposure has been linked to gut dysbiosis, increased allergies, autoimmune diseases, and obesity.
But it’s not all doom and gloom. If you must take antibiotics, pair them with probiotics and a microbiome-friendly diet. Eat fermented foods, avoid refined sugars, and give your gut time to recover. In the future, treatments like fecal microbiota transplants (FMT) may become more common to restore balance after antibiotic disruption.
Microbiome and Weight Management
Human Microbiome: Struggling with weight despite eating healthy? Your microbiome might be the missing link. Certain gut bacteria are more efficient at extracting energy from food, which means some people absorb more calories than others even if they’re eating the same thing.
An imbalanced gut can lead to insulin resistance, chronic inflammation, and hormone disruptions that make weight loss harder. For example, Firmicutes and Bacteroidetes are two dominant bacterial groups in the gut. A higher Firmicutes-to-Bacteroidetes ratio has been associated with obesity.
A diverse microbiome helps regulate metabolism, reduce fat storage, and improve satiety hormones like leptin and ghrelin. Intermittent fasting, fiber-rich foods, fermented veggies, and mindful eating habits can help restore microbial balance and promote a healthy weight.
Don’t think of your diet just in terms of calories think of it as feeding a thriving community that helps you manage your health goals.
Microbiome Testing: Is It Worth It?
Human Microbiome: With the rise in personalized health, microbiome testing has become more popular. These tests typically analyze your stool sample to give you insights into the types and proportions of microbes living in your gut. Some services even offer dietary recommendations based on your results.
While still an evolving field, microbiome testing can be a useful tool especially for those struggling with digestive issues, food intolerances, autoimmune conditions, or mood imbalances. However, it’s important to interpret the results with a grain of salt. Our understanding of what constitutes a “healthy” microbiome is still growing, and what works for one person might not work for another.
If you do decide to test your microbiome, use the results as a guide, not a diagnosis. Focus on broad principles: increase diversity, reduce processed foods, and support your gut with nourishing whole foods.
Microbiome and Chronic Diseases: The Hidden Link
Human Microbiome: If you’re dealing with chronic health issues from diabetes to autoimmune disorders your microbiome might be playing a much bigger role than you think. An unhealthy microbiome doesn’t just stay in your gut. It can affect your entire system through inflammation, immune dysfunction, and metabolic disturbances.
For instance, people with type 2 diabetes often show reduced microbial diversity and an overgrowth of inflammation-inducing bacteria. Similarly, conditions like rheumatoid arthritis, Crohn’s disease, lupus, and multiple sclerosis have all been linked to gut dysbiosis. Researchers believe that when your gut lining becomes permeable known as “leaky gut” bacteria and toxins escape into the bloodstream, triggering widespread inflammation and autoimmunity.
This isn’t just theory. Studies show that people who restore gut balance through diet, probiotics, and lifestyle changes often experience reduced symptoms or even remission of some chronic conditions. The gut is not just another organ it’s your body’s command center for long-term health.
Microbiome in Women’s Health
Human Microbiome: Women’s health is intricately tied to the microbiome, particularly in the gut, vagina, and urinary tract. A balanced vaginal microbiome dominated by Lactobacillus species keeps infections at bay by maintaining a low pH. When disrupted, women become more prone to yeast infections, bacterial vaginosis, and urinary tract infections.
Pregnancy, menopause, and even birth control can alter the microbiome. During pregnancy, for example, the gut microbiome changes to support fetal growth but if it becomes imbalanced, it can increase the risk of gestational diabetes or preeclampsia. Post-menopause, reduced estrogen can impact the diversity of the vaginal microbiota, often leading to dryness, irritation, and a higher risk of infection.
Supporting women’s microbiomes involves not only maintaining good hygiene and taking probiotics but also eating hormone-balancing foods, managing stress, and minimizing unnecessary antibiotics. It’s a whole-body system that deserves targeted care.
Microbiome and Aging: Can It Slow Down the Clock?
Human Microbiome: As we age, our microbiome naturally changes but not always for the better. Older adults tend to have lower microbial diversity, which is associated with increased frailty, inflammation, and cognitive decline. A poor microbiome can also weaken immunity, making seniors more vulnerable to infections.
The exciting news? You can influence how your microbiome ages. A Mediterranean-style diet rich in fiber, healthy fats, and antioxidants has been shown to improve microbial diversity in the elderly and reduce inflammation markers. Regular exercise, staying socially engaged, and getting quality sleep also help maintain a resilient microbiome.
We can’t stop aging, but we can certainly age better and your microbes are key players in that journey.
How to Improve and Maintain a Healthy Microbiome
Human Microbiome: Ready to boost your microbiome? Here’s your actionable checklist:
-
Eat more plants: Aim for 30+ different types of plants each week.
-
Include fermented foods: Add kimchi, kefir, sauerkraut, and miso to your meals.
-
Ditch processed junk: Minimize added sugars, refined carbs, and artificial sweeteners.
-
Manage stress: Chronic stress disrupts gut function. Try mindfulness, yoga, or deep breathing.
-
Exercise regularly: Movement boosts beneficial bacteria and lowers inflammation.
-
Sleep well: Aim for 7-9 hours of quality sleep to keep your gut-brain axis in sync.
-
Use antibiotics only when necessary: And follow up with probiotics if you do.
-
Avoid antibacterial products: Over-sanitization can strip your skin and gut of good bacteria.
-
Stay hydrated: Water supports digestion and nutrient absorption.
These habits don’t just help your gut — they strengthen your entire system from head to toe.
The Future of Microbiome Science
Human Microbiome: We’re only scratching the surface of what the microbiome can do. Researchers are now exploring fecal transplants to treat gut disorders, microbiome-based cancer therapies, and even personalized nutrition based on your unique microbial signature.
As science continues to evolve, so does the promise of microbiome medicine. We may soon be able to diagnose diseases earlier, treat them more effectively, and even prevent chronic illness all by analyzing the bacteria in your body.
What’s clear is this: your microbiome is not just a passive passenger it’s an active partner in your health journey. Nurture it, and it’ll reward you in ways you never imagined.
Conclusion
Human Microbiome: The human microbiome isn’t just a health trend it’s a revolution in how we understand our bodies. These trillions of microbes play a vital role in digestion, immunity, mental health, weight management, and even how we age. With every bite you eat, product you use, or lifestyle choice you make, you’re influencing your inner ecosystem.
The beauty of the microbiome is that it’s dynamic. You can change it, improve it, and optimize it for better health. Start small, be consistent, and remember you’re never alone. You’ve got trillions of microscopic allies rooting for your well-being.
FAQs
Q1. Can I take probiotics daily?
Yes, most people can benefit from daily probiotics, especially if they eat a low-fiber or highly processed diet. Just choose a high-quality supplement and combine it with a plant-rich diet for best results.
Q2. How long does it take to restore gut health?
With consistent diet and lifestyle changes, improvements can begin in just a few days, but full restoration of microbiome balance may take several weeks to months.
Q3. Do antibiotics permanently damage the microbiome?
Not always, but they can cause long-term imbalances if overused. Recovery is possible through diet, probiotics, and time.
Q4. Is a diverse microbiome always better?
Generally, yes. Diversity increases resilience and supports better health outcomes. However, diversity alone isn’t everything the presence of specific beneficial strains is also important.
Q5. Can kids benefit from microbiome support?
Absolutely. Early microbial exposure is essential for immune development. Encourage outdoor play, a varied diet, and limit unnecessary antibiotics for children.